TEFCA: Framework and Common Agreement Version 1 Released!

On Tuesday, January 18, 2022 ONC and the RCE released the first official version of the Trusted Exchange Framework and Common Agreement – TEFCA.
We’ve covered TEFCA quite a bit in the past (TEFCA in a Nutshell, TEFCA in a Nutshell – Part 2, Newsflash: TEFCA Anticipated to be LIVE in 2022!, TEFCA: Update for 2022) so we won’t cover the basics again in this blog post. Rather, we’ll take a look at how TEFCA might affect healthcare providers and organizations, and offer some thoughts on how TEFCA may shape interoperability over the next few years.
Sustainability: The Key Challenge for TEFCA?
As some may remember, the HITECH Act included “Beacon” grants, which provided $220 million to support the development of Health Information Exchange (HIE) capabilities across the country. While this was successful in starting many new HIEs, ultimately once the Federal funding ran out many HIEs failed, as they did not have an adequate secondary source of funds to support their long-term viability.
Fast forward a dozen or so years, and TEFCA is now facing the same situation–how will TEFCA and the RCE generate sufficient revenue to cover its costs, and provide a sustainable HIE infrastructure?
What we’ve learned from the Common Agreement is that QHINs (Qualified Health Information Networks) will be required to pay fees to the RCE (the Recognized Coordinating Entity, namely the SequoiaProject). Further (and not unexpectedly) these fees may be updated by the RCE from time-to-time as necessary to cover their costs. While specific fees are referenced in the Common Agreement as part of “Schedule 1”, this schedule has to date not been included with the Common Agreement materials.
QHINs however, are not allowed to charge other QHINs for any exchange of information using the Connectivity Services. However QHINs are allowed to charge Participants fees (with Subparticipants potentially paying those fees as a pass-through). How these are structured however, will be determined by each individual QHIN.
TEFCA: Financial Benefit or Detriment to Hospitals?
Consider then the case of a hospital or health system that is currently connected to multiple HIEs, perhaps 6 or more as is the case for some states, and where fees are often charged to hospitals in order to connect with these various HIE organizations.
With TEFCA, Participants and Subparticipants will be able to choose their QHIN based on the services provided and fees charged. Hospitals, Health Systems, and even Providers may connect directly to a QHIN, or may connect to TEFCA as a Subparticipant (perhaps connecting through another Health Information Exchange).
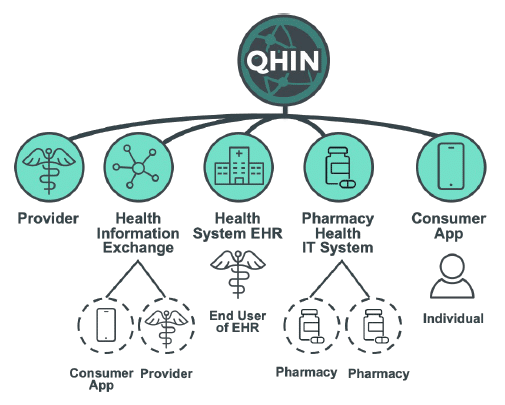
Source: Common-Agreement-Users-Guide.pdf
Given that information exchange services will be uniform for all QHINs as governed by the Common Agreement, (with the possible exception of Individual Access Services (IAS)) then it would seem that Participants and Subparticipants might choose the least expensive option.
Consequently, unless state or regional HIEs can offer additional services (e.g. perhaps membership rosters and care coordination for Population Health) then it is possible that organizations might be better off with a single connection to a QHIN (or perhaps to a single Participant HIE) rather than to maintain multiple separate connections as they do now.
One wonders then whether the financial realities of TEFCA will ultimately lead to fewer HIEs, and a more centralized interoperability landscape? Indeed, will state and regional HIEs become superfluous, with most organizations connecting directly to a TEFCA QHIN? Regardless, it seems likely that regional HIEs will be facing increasing market pressure in the future.
Alternatively, if the fees required to support the QHINs are significantly higher than current costs for healthcare organizations (and there is significant discussion for example regarding the costs required of the QHINs to support the RCE Directory Services), then TEFCA may potentially prove to be more expensive for Participants and Subparticipants.
Ultimately the answer to these questions will be determined by the actual costs associated with the program, the costs charged to the QHINs by the RCE, and how costs are levied to Participants and Subparticipants–all key elements of a viable sustainability plan for each QHIN, and the key challenge for TEFCA going forward.
FHIR: The Future of TEFCA?
Perhaps the most interesting and significant announcement as part of the release of TEFCA is the support by ONC for FHIR in the future by publishing a FHIR Roadmap and timeline for implementation.
“The goal is to include FHIR as an optional, additional standard in the QTF in CY 2023 for those ready to use it, and to gradually make it a required, additional capability during CY 2024.”
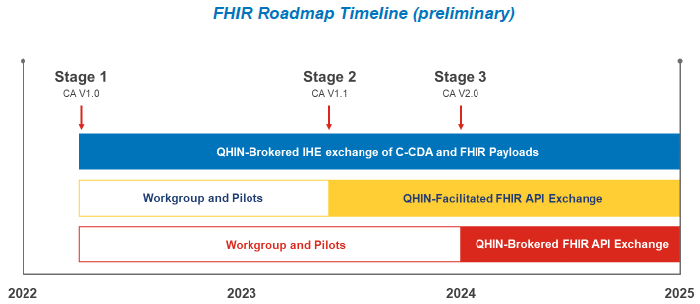
Source: FHIR Roadmap v1.0_updated.pdf
Two types of exchange are anticipated to be supported:
QHIN-Facilitated Exchange: where QHINs facilitate unbrokered FHIR API-based exchange between Participants and Subparticipants from different QHINs.
QHIN-Brokered Exchange: where QHINs broker FHIR payloads by routing FHIR APIs transactions between Participants and Subparticipants from different QHINs.
QHINs will be required to support network-brokered IHE exchange and may optionally support network-facilitated FHIR API exchange.
Many have asked for clarification from the RCE on their plans for FHIR, and this roadmap clearly addresses those questions. Like other regulatory programs such as MIPS/MACRA and Information Blocking, it seems TEFCA views FHIR as the future of Interoperability.
Certainly as TEFCA matures it is likely that FHIR will become an increasingly important component of the HIE ecosystem. We’ll be watching closely to see how the relationship between FHIR and TEFCA evolves–2024 can’t come soon enough!
Helpful Links
HIMSSCast Podcast
How Health Systems Can Prepare for TEFCA
Common Agreement Version 1
- https://rce.sequoiaproject.org/common-agreement/
- Zip file: https://rce.sequoiaproject.org/wp-content/uploads/2022/01/CA-Resources.zip
- QHIN Technical Framework: https://rce.sequoiaproject.org/wp-content/uploads/2022/01/QTF_0122.pdf
RCE (Sequoia Project)
- https://rce.sequoiaproject.org/
- RCE FAQ: https://rce.sequoiaproject.org/rce/faqs/
- Webinars: https://rce.sequoiaproject.org/community-engagement/

























