Demands and Expectations from Multiple Stakeholders in Healthcare: Actionable Strategies for 2023

Providers simultaneously need to improve employee retention and development, address clinician burnout, respond to rising consumerism – while also bettering their understanding of social determinants of health (SDOH) and the unique needs in their community. Many key strategic initiatives underway today require engagement from multiple stakeholders.
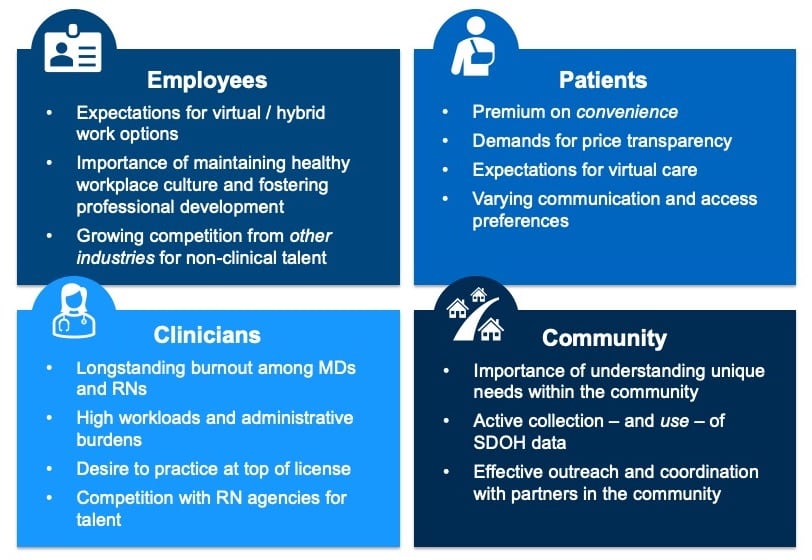
Hospitals and health systems increasingly need to strive for a more holistic and cohesive stakeholder experience, understanding – and accounting for – the specific pain points, perceived inefficiencies, and unique frustrations of each stakeholder in a given initiative. For example, telehealth programs are evolving across the country, with leading health systems focusing on centralizing governance and ensuring alignment between the virtual care program and the organization’s overall strategic goals. A key element of that evolution though (which is sometimes overlooked) is carefully considering the patient and the clinician “virtual care experience” – and adapting accordingly.
Success with Virtual Care Requires Focus on the Patient and the Clinician Experience
Per a recent NEJM Catalyst survey of U.S. clinicians, clinical leaders, and health delivery executives:
-
Only 55% said their organization measures “patient experience for telemedicine care”
-
Only 39% said their organization offers “either an internal or external training program for telemedicine [for clinicians]”
Similarly, efforts by hospitals and health systems to better understand and address unique needs in their community are increasingly prevalent. While success with SDOH-related initiatives requires effective outreach and coordination with local stakeholders (e.g., community-based organizations, social services agencies, public health institutions, payers, etc.), efforts to raise awareness internally and provide clinicians with education about the programs underway are just as important. For example, when physicians were asked about challenges impacting their time and ability to address their patients’ SDOH, two of the top four responses were “community resources not available, inadequate or difficult to access” and “inadequate information about availability / access to community resources.”
“Please rate the impact of each of the following, if any, on your time and ability to address your patients’ SDOH.”
n=1,502 physicians
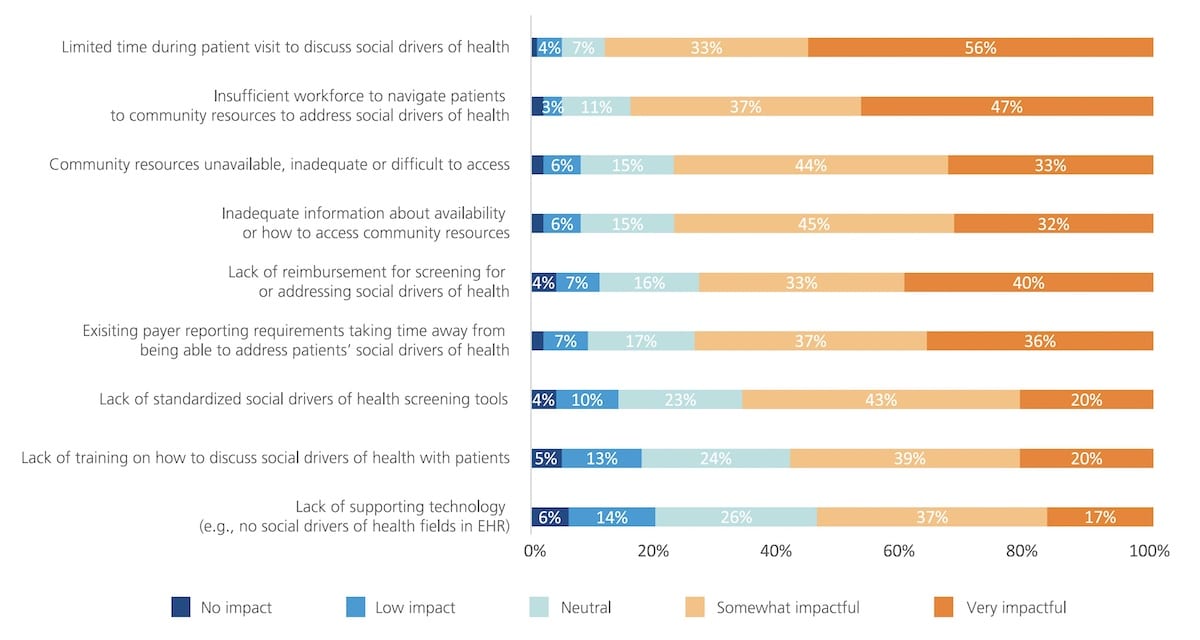
Source: “2022 Survey of America’s Physicians: Part 1 of 3,” The Physicians Foundation, Mar 2022
Actionable Strategies
-
Leverage tools and data to understand specific pain points, frustrations, and concerns among non-clinical employees, clinicians, and patients.
-
Invest in market research and collect data at every step in the patient journey.
-
Invest in customer relationship management (CRM) capabilities to support new patient acquisition, patient service, marketing campaign initiatives, and physician relationship management.
-
Take a human centered design approach to technology solutions and ensure all relevant stakeholders are considered during decision-making.
-
Be agile and flexible to adapt to ever-changing needs.
-
Focus on the 3 Cs: Communication, Change Management, and Culture.

























