The hospital-at-home initiatives launched by health systems to date often have evolved organically out of need, commonly citing capacity problems. The value proposition of a hospital-at-home may simply not be there for a health system that isn’t facing a severe bed shortage. Capitalizing on the potential value from a hospital-at-home also hinges on having a large volume of patients – specifically patients with the types of conditions that are taking up hospital beds – who can be transitioned to a home setting. For some health systems, this may only represent a small fraction of the patient population, as patients need to be sick enough to require inpatient-level services but stable enough to be cared for in their home. Every health system’s patient population will be different, but common conditions treated via hospital-at-home initiatives include pneumonia, congestive heart failure, COPD, cellulitis, and COVID.
Does a Hospital-at-Home Make Sense for Your Health System

Despite continued interest among providers, the reality is the hospital-at-home is not currently a fit for every health system. Before moving forward with a hospital-at-home – or any new initiative with a telehealth or virtual care component – health systems should have a plan in place to understand and refine their existing virtual care processes, capabilities, and controls. There are five key questions that any provider organization should carefully consider.

Hospital-at-Home Background and Core Components
As virtual care continues to evolve and is now a staple of care delivery, the hospital-at-home, a hybrid virtual / in-person care model where inpatient level services are provided in a patient’s home, is transforming care. The concept is by no means new, but interest in developing formal hospital-at-home initiatives was rekindled during the pandemic as a way to alleviate capacity issues while also limiting transmission of the virus. The launch of CMS’ Acute Hospital Care at Home program in 2020 allowed providers to apply for waivers of the requirement for “nursing services to be provided on premises 24 hours a day, 7 days a week.” The program was recently extended through the end of 2024. As of 4/27/23, there were 124 health systems (representing 278 hospitals) in 37 states that had been approved for a waiver.
It is important to note the “hospital-at-home” is a concept whereas “Acute Hospital Care at Home” is a specific program from CMS that allows providers to receive reimbursement for delivering inpatient level care in a Medicare beneficiary’s home. The hospital-at-home concept has been around for decades – and there are many hospital-at-home initiatives underway today that significantly pre-date the pandemic. Given that reimbursement has long been the biggest barrier to scaling hospital-at-home initiatives, the launch – and subsequent extension – of CMS’ program was a logical catalyst in terms of generating more interest among providers. But the hospital-at-home is much broader than the program from CMS – and many of the organizations who implemented a hospital-at-home to care for COVID patients are now looking to build on their experience and expand.
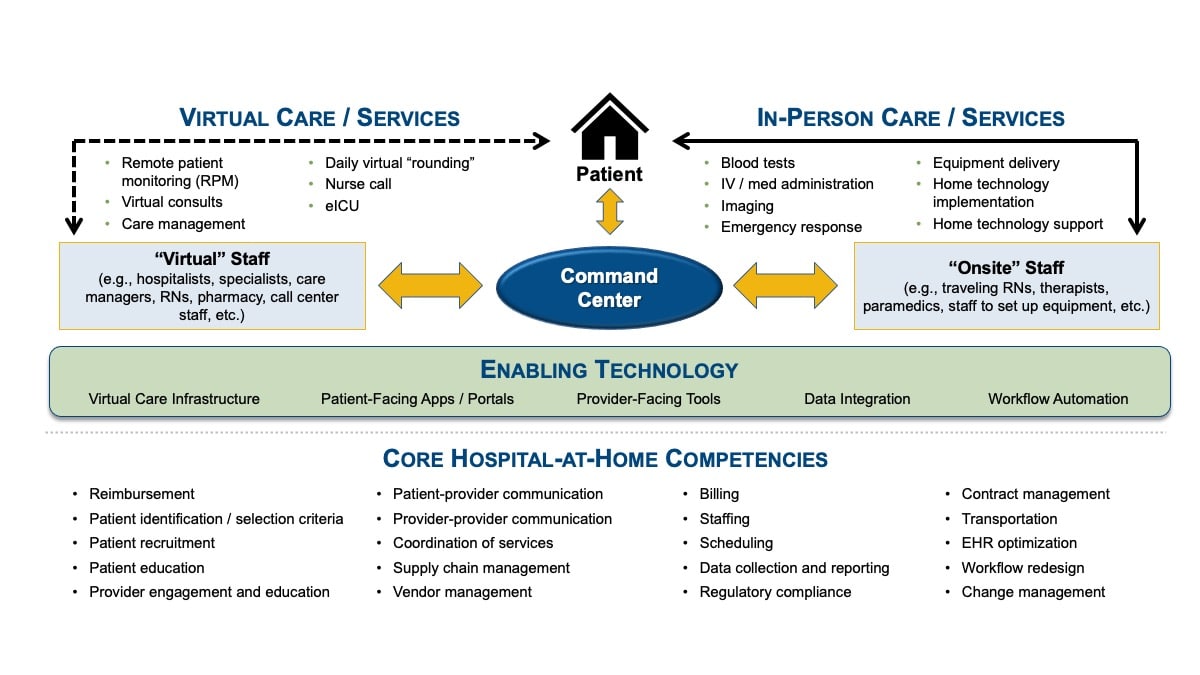
While each hospital-at-home will inherently be somewhat different, there are three essential components for any initiative.
Hospital-at-Home Framework
Five Questions to Ask
Although the hospital-at-home has generated considerable interest among providers, the reality is the model is not a fit for every health system. There are five key questions that any provider organization should carefully consider before moving deciding to move forward with a hospital-at-home initiative:


The unique market characteristics for a provider organization are an important factor. There will be different considerations depending on the local infrastructure, new market entrants, competitive pressures, and their service area’s baseline social determinants of health (SDOH). For example, the in-person aspect of the hospital-at-home means that daily nurse visits need to be logistically feasible (e.g., time, travel, and costs), while the telehealth component of the model means reliable internet access in the home is essential for services like remote patient monitoring (RPM) and virtual patient-physician consults.

Reimbursement has historically been the biggest barrier to achieving scale with hospital-at-home initiatives. The recent extension of CMS’ Acute Hospital Care at Home program through the end of 2024 is certainly welcome news, but it is important to remember the reimbursement applies only to Medicare beneficiaries. Health systems also need to be capable of meeting any quality and reporting requirements associated with hospital-at-home programs they are participating in – requirements that are likely to continue to evolve over time. This means not only collecting the right data needed for quality reporting, but also actively monitoring key performance indictors (KPIs) and having the right interventions in place to improve care.

Given the complexity and sheer scope of core competencies required for a successful hospital-at-home, experience is paramount. Health systems best positioned to succeed with the model are those with an existing home health offering in addition to robust telehealth capabilities. Having virtual care offerings currently in place that include a centralized command center (i.e., an in-house RPM initiative or an eICU) are particularly valuable, as the health system can leverage that personnel experience, institutional knowledge, and infrastructure for the hospital-at-home.
Even health systems with significant experience in the underlying core competencies required for a hospital-at-home will still likely need to strategically position partners and capabilities to enhance their offerings. This is especially true as needs change when trying to get the initiative to scale.

Telehealth is now firmly entrenched as a part of the overall foundation of heath delivery. Now that the federal Public Health Emergency (PHE) has expired, providers can expect their virtual clinical services to undergo the same level of scrutiny that their in-person clinical services receive. The fact that HHS’ Office of Inspector General (OIG) published a “toolkit” in April 2023 to provide payers with “detailed information on methods to analyze telehealth claims to identify program integrity risks associated with telehealth services” speaks volumes. The document states bluntly: “…along with the dramatic increases in [telehealth] use there have been concerns about fraud, waste, and abuse. Most recently, as part of the extension of telehealth in Medicare, lawmakers highlighted the need for further study on telehealth and Medicare program integrity.” In other words, more oversight and audits of virtual care efforts are expected in the coming years.
As a result, before launching a hospital-at-home – or any new initiative with a virtual care component – health systems need to carefully review their current telehealth processes, capabilities, and controls for billing compliance (e.g., coding, documentation, and licensing / telehealth registrations).
The Bottom Line
Anything other than a resounding “yes” to the five questions above should give a health system pause before embarking on efforts to build a hospital-at-home. However, just because the hospital-at-home isn’t a fit for your health system doesn’t mean the model is not something to consider in the future, especially as reimbursement evolves, your needs change, and industry experience with the concept becomes more widespread.
The hospital-at-home ultimately represents just one type of care model that involves virtual care. There may be other virtual care initiatives (and even other hybrid virtual / in-person initiatives) worth pursing that are more closely aligned with your organization’s unique strategic priorities and which represent a better fit for the realities in your market. However, before moving forward with any new initiative with a significant virtual care component – or even before expanding on existing virtual care offerings – it is essential that your health system has a plan in place to understand and refine your existing telehealth processes, capabilities, and controls.
Contributors:
Jay Backstrom, Practice Leader
Bryan Arkwright, Principal
Related Articles:
Determining the Value-on-Investment of Provider-to-Provider Virtual Consultation for Cancer Care
























