3 Elements for Successful Workforce Management: Embracing a New Way of Thinking in Health Delivery

Rising labor costs – driven by increased staff turnover, growing use of external agency labor, and demand for higher wages – continue to account for a large percentage of hospital and health system expenses. Although the problem is evolving, the approaches to measuring and managing labor in health delivery remain antiquated, plagued by 1) financial performance targets that are misaligned with workforce management tools, 2) a lack of understanding among front-line managers about the dynamic relationship between hours, volume, and cost, and 3) the lack of discipline and rigor around labor expense management processes, cadence, and reporting.
In the current environment, effective workforce management requires hospitals and health systems to embrace a new way of thinking centered on patient-focused staffing; one that empowers front-line managers to run their departments as if they were small businesses.
There are three elements to a successful program.
Leveraging data that is aligned with patient-focused staffing.
The first step in optimizing hospital and health system workforce – and maximizing productivity – is ensuring key operational and clinical stakeholders have access to the data that can best support informed decision-making. The traditional way of measuring labor in health delivery is woefully inadequate. The data that many hospitals and health systems currently rely on to make workforce decisions is far too one-dimensional, disproportionately focused on hours worked without enough consideration for the inherent variances in patient demand and the inextricable relationship between hours, volume, and cost. The result is that health delivery organizations today end up just staffing to a schedule instead of to patient needs. Additionally, focusing solely on worked hours per unit of service (WHPUOS) doesn’t factor in the critical aspect of costs.
New Way of Thinking
Impact Advisors works with our clients to establish labor productivity targets that are not only based on WHPUOS, but paid hours per unit of service (PHPUOS), and cost per unit of service as well – which collectively provide alignment with true cost, overall budget, and patient needs.

Strategically utilizing the right combination of labor reports and interactive tools.
Just like the act of wearing a heart monitor doesn’t automatically make a person healthy, simply having a system in place to measure performance doesn’t mean an organization is effectively managing their workforce. The right reports and tools are essential to ensure front-line managers are using data to take the appropriate actions. There is an important difference between reports and tools. Reports reflect current performance, whereas tools provide the roadmap for reaching the desired performance level. Both are critical for ensuring the organization is appropriately staffing to meet the needs of patients, but they need to be used strategically. In other words, for each report and/or tool, there needs to be a robust methodology for when to use it, where to use it, who uses it, and how they use it. The rigor and cadence are important.
New Way of Thinking
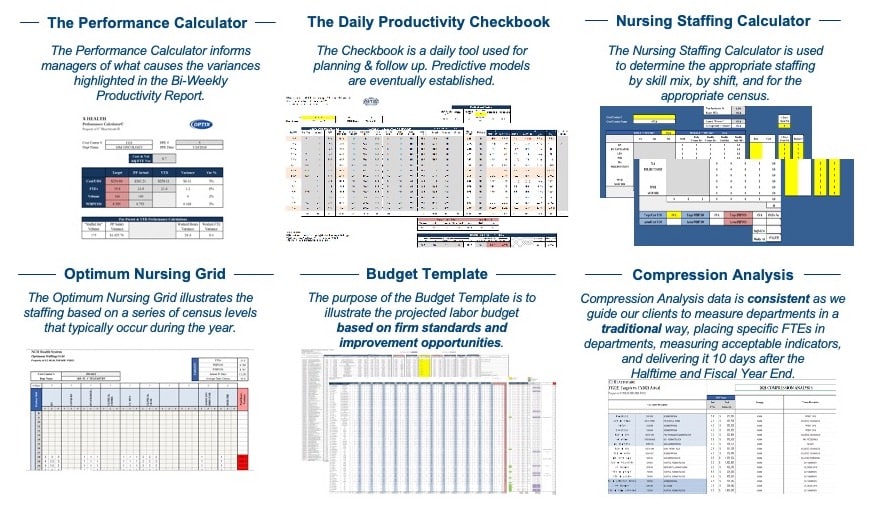
Impact Advisors has a variety of labor productivity reports and tools, each designed to be relevant for a specific phase in the workforce management process.
Examples of Impact Advisors’ OPTIX Labor Productivity Reports

Examples of Impact Advisors’ OPTIX Labor Productivity Tools
New Way of Thinking
Impact Advisors’ OPTIX reports track progress against a wide range of metrics at the organizational and department level to give clients an accurate and holistic view of current workforce performance. Meanwhile, our tools – which provide the roadmap to reach targeted performance levels – are dynamic and interactive, allowing front-line managers to look at how certain changes to their staffing model will impact productivity and costs given likely fluctuations in patient volume, staff turnover, and department vacancies. This enables managers to be more proactive with hiring and staffing decisions, saving money by preventing situations of the organization being caught flat-footed by (ultimately predictable) staffing shortages and then having to turn to expensive third-party agencies at the last minute to fill urgent needs.

Providing education, ensuring engagement, and driving cultural change
Establishing labor productivity targets that accurately reflect the dynamic relationship between hours, volume, and cost and leveraging the right reports and interactive tools that can serve as a roadmap to reach those targets are crucial, but ultimately still represent only part of the equation. There also needs to be a strong and continuous organizational commitment to engaging and educating department leads and driving cultural change. The reality is that most front-line managers in health delivery today don’t have a solid understanding of what goes into the information they see in labor reports. They’ve historically been trained to simply “read” the reports they are given without being offered any training on the factors that influence the metrics for which they are responsible.
New Way of Thinking
It is virtually impossible to foster an environment of fiscal accountability and continuous improvement if the people responsible for meeting a labor productivity target have no idea what is driving the data shown in their reports. This usually leads to denial of the targets or massaging the data to look more favorable by carving out hours, normalizing hours, or rolling departments up. This is why Impact Advisors wraps coaching and education around our reports and tools. As part of our Engagement Process, we teach front-line managers how to interpret data and how to influence it, whether from an hours perspective, a volume perspective, or a cost perspective. One aspect of our Engagement Process is productivity huddles, which offer a platform to review prior pay period performance, understand the root cause of productivity variances, and identify solutions that combat these variances.

The Bottom Line
Workforce pressures in health delivery are not going away any time soon. Hospitals and health systems need to abandon the outdated approaches currently in place for measuring and managing labor – and embrace a new way of thinking that empowers front-line managers to run their departments as if they were small businesses. Success in the current environment requires leveraging data that is aligned with patient-focused staffing, strategically and deliberately utilizing the right reports and interactive tools, and perhaps most importantly, providing regular coaching and education.
Contributors:
Dave LeClercq, Practice Leader
Harnish Patel, Director
Related Article:
























