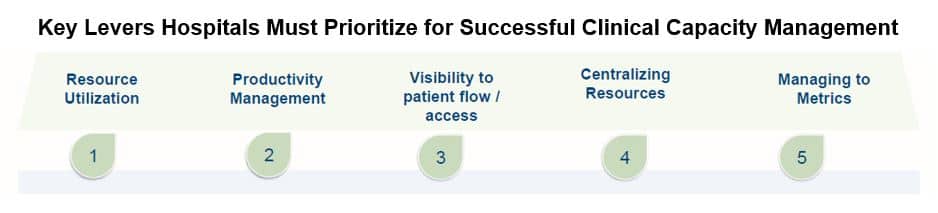
Five Key Levers that Drive Clinical Capacity Management Transformation

Overcrowded ERs, longer lengths of stay (LOS), and workflow inefficiencies continue to plague hospitals, creating care gaps, patient dissatisfaction, and higher costs. To solve these problems, health delivery organizations need to focus on clinical capacity management and embrace tactics that strategically address demand and patient flow with a combination of clinical processes, technology, and resources.
Clinical Capacity Management: Five Levers Hospitals Must Prioritize
We define clinical capacity management as “the practice of achieving command of your resources to optimize and maximize patient access and organizational ability to improve the quality of care.”
1. Resource Utilization
An important tactic for achieving effective resource utilization is ensuring clinicians work at the top of their license. Nurse managers and directors need to look at how their team is configured and understand potential resource challenges at any given time – and then have the operational agility to re-engineer the workday to best promote clinical capacity management. Mindful and deliberate use of resources is key. For example, as part of the discharge process, a nurse will often accompany a patient to the exit to ensure they transition safely to a car, but that round trip can take 45 minutes or more. By making better use of in-house transport resources to escort patients out of the hospital, nurses are able to spend more time on the unit and can quickly move on to delivering care to the next patient.
Another key tactic is optimizing technology and ensuring alignment between the enterprise electronic health record (EHR), the hospital’s resources, and evidence-based information. For example, embedding the critical tasks that are part of the care pathway for specific disease conditions into the EHR – and then sending bedside nurses a best practice alert if a given action has not taken place within a certain period of time.
2. Productivity Management
Although most nurses understand productivity from a conceptual perspective, hospitals and health systems have historically provided little help to frontline staff when it comes to understanding how productivity metrics are calculated and which factors can influence the productivity targets to which they are held accountable. The right training and education are essential, so leaders are empowered to manage their unit from a clinical and business perspective.
Clinical leaders need to foster a culture that keeps the frontline nursing team’s focus on improving outcomes, patient and clinician experience, and lowering costs. Productivity targets cannot be viewed as “just a number”; instead, improving productivity should be seen across the clinical team as a vehicle to providing quality care to more patients. Frontline staff need access to actionable data, but metrics and targets are most powerful when team members keep the organization’s mission – and their calling as clinicians – front and center.
3. Visibility to Patient Flow / Access
While technology can increase line of sight to barriers related to patient flow and access to care, it should be implemented thoughtfully. There is a propensity to enable every alert in the EHR, which only exacerbates the longstanding problem of alert fatigue among clinicians. Organizations should invest the time to review and prioritize automated notifications and focus on enabling alerts that are directly tied to driving top-tier performance and clinical quality. For example, implementing a visual cue in the EHR or bed board to indicate a patient is clinically ready to leave the hospital but has a psychosocial barrier that needs to be addressed before they can be safely discharged.
Increasing situational awareness is critical for ensuring a line of sight to patient flow and access issues. Frontline nurses need to understand when there is a shortage of resources or a sudden surge in demand, and how to respond. Technology is an invaluable tool, but there is no substitute for bringing the team together for a daily “huddle” to discuss the challenges of the day and review an action plan.
4. Centralizing Resources
Hospitals should consider centralizing or co-locating resources when it makes sense. Managers and directors need to understand how resources are currently being used and which types of shared resources are available on a given day. Clinical leaders should ask questions such as: “Have we leveraged opportunities such as virtual sitters? Are we centralizing our telemetry monitoring team? Have we maximized use of centralized telehealth services for certain patient populations to offload pressures on the emergency department? Are we automating as much as possible to reduce the workload of frontline nurses?”
5. Managing to Metrics
Performance and outcome data must be transparent and customized, so the frontline team members can easily understand their role in responding to anomalies or situations that require action. Data should also inform how the organization designs (or reengineers) the day-to-day hospital workflow in a way that focuses on strategic priorities while accounting for variances in demand and patient flow.
One often overlooked – but critical – aspect of managing to metrics is simply investing the time upfront. Hospitals need to be thorough and deliberate to ensure any data that informs key performance metrics has been fully validated and is being pulled from the right sources. It needs to reflect true performance against a given target and drive an understanding of tangible opportunities for improvement.
The Bottom Line
The problems of overcrowded ERs, longer lengths of stay (LOS), and workflow inefficiencies are unlikely to subside any time soon. To address the care gaps, patient dissatisfaction, and higher costs already rampant in health delivery, hospitals and health systems must embrace clinical capacity management.
The Impact Advisors Difference – Clinicians Who Know Tech
Impact Advisors has the clinical and technical expertise to help widen the front door, improve the continuum of care, and optimize workflows (and automate where appropriate). We listen, respond with empathy, and challenge with respect because we’ve been there. Our clinical experts understand the workflows because they’ve performed them while serving in the same clinical roles. They also know the EHR systems better than most and are backed by the firm’s collective knowledge gleaned over 15 years as the industry’s top EHR implementer.
Learn more about our clinical optimization capabilities.

























